

Period prevalence of uveitis in human T-lymphotropic virus 1 carriers versus noncarriers in a highly endemic area: The Nagasaki Islands Study
An original article by Assistant Professor Jun Miyata, et al. (Department of Island and Community Medicine, Graduate School of Biomedical Sciences), was published in May 7, 2024 (online ahead of print).
Background
Human T-lymphotropic virus 1 (HTLV-1) is a retrovirus that is likely to persist via clonal expansion in the chronic stages of infection, leading to multiple HTLV-1-associated diseases, such as adult T cell leukemia, HTLV-1-associated myelopathy/tropical spastic paraparesis, and uveitis. Uveitis is an inflammatory disorder that affects intraocular tissues and causes ocular symptoms, such as floaters, blurred vision, ocular pain, photophobia, and burning. Although HTLV-1-associated uveitis is an accepted clinical entity, the magnitude of the risk of uveitis in HTLV-1 carriers compared with that in non-carriers remains to be investigated. Therefore, the authors aimed to compare the risk of uveitis in HTLV-1 carriers with that in non-carriers, based on data from a population-based cohort study in a highly endemic area of HTLV-1 (Nagasaki) in Japan.
Methods
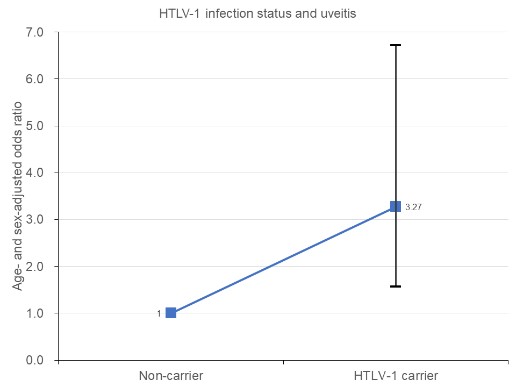
The study included 4,265 residents (men, 39.2%), mostly middle-aged and older individuals with a mean age of 69.9 years, who participated in the surveys between April 2016 and September 2022. HTLV-1 carriers were identified by screening using chemiluminescent enzyme immunoassays and confirmatory tests. Participants with uveitis were determined from the medical records of all hospitals and clinics where certified ophthalmologists practiced. Logistic regression analysis in an age- and sex-adjusted model was conducted to compute the odds ratio (OR) and 95% confidence interval (CI) of uveitis according to HTLV-1 infection status.
The 6.5-year prevalence of uveitis was almost three-fold higher among HTLV-1 carriers.
Thirty-two (0.8%) participants had uveitis. For HTLV-1 carriers, the age- and sex-adjusted OR (95% CI) of uveitis was 3.27 (1.57–6.72) compared with non-carriers.
Conclusions
HTLV-1 infection was associated with a higher risk of uveitis among mostly middle-aged and older Japanese individuals living in areas highly endemic for HTLV-1. The 6.5-year prevalence of uveitis was almost three-fold higher in HTLV-1 carriers than in non-carriers. The findings suggest that physicians who treat HTLV-1 carriers should assess ocular symptoms to avoid not detecting uveitis, and that those who diagnose patients with uveitis should consider HTLV-1 infection.
Prior studies into the pathogenesis of HTLV-1-associated uveitis have stated that accumulated HTLV-1-infected T cell-stimulated inflammatory cytokines in the eye can damage ocular tissues, HTLV-1-infected retinal pigment epithelial cells can disturb immune homeostasis in the eye, and epitopes of HTLV-1 antigens can cross-react with retinal antigens.
These results were consistent with the findings of prior studies. The limitations of this study include the influence of participants’ death or loss to follow-up from the cohort study during the study period and the inability to calculate the cumulative incidence of uveitis because some cases were prevalent at the time of exposure measurement and could not be distinguished from new cases. Therefore, validation of these findings is necessary.
Reference
URL: https://onlinelibrary.wiley.com/doi/full/10.1002/jmv.29653
DOI: 10.1002/jmv.29653