

A noninvasive test for human prion disease using hair roots and scalp
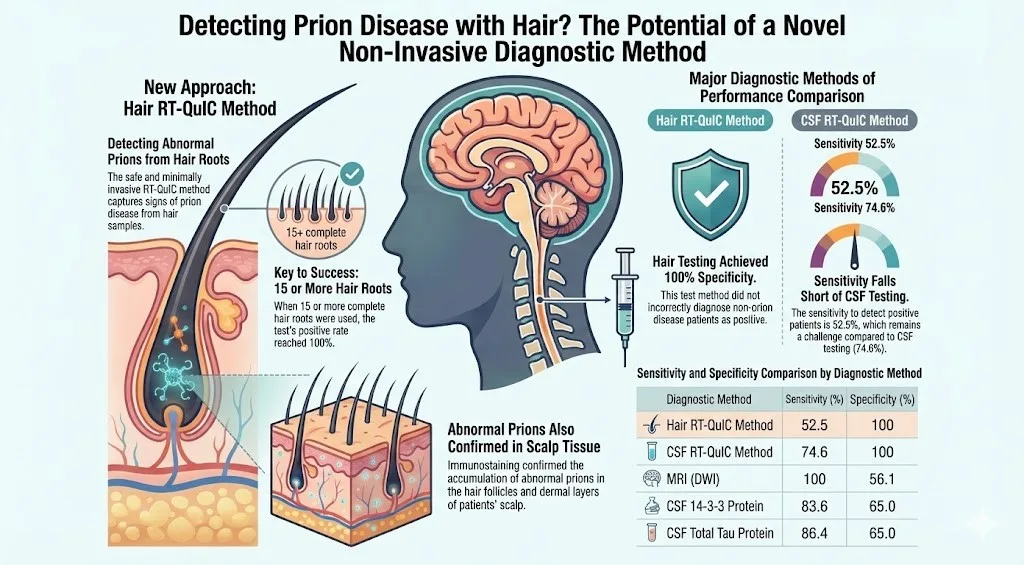
A research group led by Professor Katsuya Satoh at the Nagasaki University Graduate School of Biomedical Sciences has verified the efficacy of a novel non-invasive approach for detecting Prion Seeding Activity (PSA) from hair roots and scalp tissue. This method utilizes the Real-Time Quaking-Induced Conversion (RT-QuIC) assay—a technology developed at Nagasaki University that is already instrumental in the diagnosis of Human Prion Disease (HPD). While the conventional RT-QuIC method using cerebrospinal fluid (CSF) demonstrates exceptional accuracy (Sensitivity: 80–90%; Specificity: 99–100%), CSF collection is an invasive procedure that imposes a significant burden on patients. This study suggests the potential for a safer, non-invasive diagnostic alternative using samples such as hair roots and scalp skin, which can be obtained via routine grooming activities like brushing or from bedding.
1. Verification via Autopsy Cases In an analysis using RT-QuIC on scalp and hair roots collected from 22 autopsied HPD patients, PSA positivity was confirmed in 100% of cases. Pathological examination revealed abnormal prion proteins in hair follicles, granulation tissue, and keratinocytes within the dermis layer. Notably, the study revealed that PSA levels in the scalp exhibit seeding activity similar to that found in brain tissue.
2. Prospective Study Results In a prospective study involving 177 HPD patients and 123 non-HPD patients, the hair root RT-QuIC method yielded a sensitivity of 52.5% and a specificity of 100%.
3. Sampling Requirements and Disease Type Variance The study indicated that collecting 15 or more completely intact hair roots is necessary to ensure 100% positive results; samples lacking roots resulted in very low positivity rates. Furthermore, sensitivity varied by disease subtype:
4. Clinical Implications Hair root RT-QuIC offers a promising non-invasive diagnostic alternative for patients who cannot tolerate lumbar puncture due to conditions such as severe spinal deformity or intense myoclonus. To advance this method toward clinical implementation, comprehensive validation studies using larger patient cohorts and appropriately matched control groups are essential.
Non-invasive Refers to medical procedures that do not break the skin or physically enter the body. These methods cause minimal to no physical burden or pain to the patient (e.g., avoiding incisions or needle insertions).
Sensitivity The ability of a test to correctly identify those with the disease (true positive rate).
Specificity The ability of a test to correctly identify those without the disease (true negative rate).
Autopsy A post-mortem surgical examination of a body to determine the cause of death or pathology.
Keratinocytes The primary type of cell found in the epidermis (the outermost layer of the skin), playing a key role in protecting the body from environmental damage.
Prospective Study A longitudinal study that follows a group of individuals over time. Participants are divided based on exposure to certain factors, and the study tracks the development of outcomes (such as disease) into the future.
Myoclonus Sudden, involuntary jerking of a muscle or group of muscles. It can occur in various parts of the body (limbs, face, trunk) without loss of consciousness.
Cohort A group of individuals who share a defining characteristic, observed over a period of time in a scientific study.